When you arrived at work this morning, were you worried that a police officer might be waiting for you? Horrible start to the day, that, seeing a uniformed officer blocking your way. Inside, you see other officers taking copies of all your computer files and emails. The officer speaks gently, but firmly. Come with me please. Yes, your manager has been informed. Now, please, if you would.
I really hope this never happens to you. But it could. Because passing through Parliament at the moment is the Care Bill, and it creates new criminal offences that will affect anyone who works with waiting lists or patient coding, including information analysts, clerks, clinicians and managers.
Check it out for yourself. It’s all in Section 81 and there’s plenty of background in the Department of Health’s Impact Assessment (IA).
The proposed offence is to supply false or misleading information, and because this is a criminal offence it involves the police, Crown Prosecution Service and courts. It applies to care providers not individuals, so nobody will go to jail but the fines, remedial orders, and publicity orders will be heavy enough.
We don’t yet know exactly what kinds of information will be covered because those will be specified in regulations, but the IA makes clear that mortality rates and waiting times data are top of the list (and in this post I will deal only with the waiting list aspects). And what if the data error is an honest mistake? It that case “it is a defence for a care provider to prove that it took all reasonable steps and exercised all due diligence to prevent the provision of false or misleading information”.
This is tough stuff. Is it a good thing? Yes. Waiting list data is a clinical safety issue. If patients get lost in the system, then they are at risk. If every report of a long-waiting urgent patient is met with “oh, that must be a data error”, then the genuine cases will not be caught quickly and patients will come to harm. The NHS has tolerated high levels of data error on its waiting lists for its entire existence and it is time that stopped.
But I think the Department of Health is wrong, in its Impact Assessment, to expect that a dozen or so hospitals will face police action every year. That would be a failure: a failure to change the culture of top-down control and punishment, as well as a failure of the local NHS to clean up its data. The purpose of the criminal law is not to performance-manage the bottom 5 per cent of hospitals; it is there to deal with crime. If the police have to bring charges under this section (for waiting list offences) more than once every few years, then that is too many.
What do we need to do, to avoid the drip, drip, drip of regular police investigations and prosecutions? Due diligence, yes, but that is only the means: accurate waiting list data is the end, and we need to keep that end clearly in sight. This is going to be a big but worthwhile job, and it is going to involve hundreds of people in every NHS Trust. If everybody is focused on covering their backs with audit trails (instead of making patient records accurate) then it will all be an expensive waste of time.
Let’s start with the fundamentals. Mainstream administrative records should reflect accurately the real patient journeys that are taking place in the hospital. The patient is referred from outside, waits, is seen by a clinician, is perhaps referred to another clinician (and waits again), and so on until eventually the patient is discharged. Each stage of that pathway may involve a different IT system, and ultimately we want each system to record and report where the patient came from and why, where they went next and why, or (if they haven’t gone anywhere yet) how they are currently being managed.
It’s like a bank account. Every penny is accounted for: where it came from, and where it went, or (if it’s still there) which account it’s in. And the accounting analogy turns out to be very useful, because we can check that our bank statement is correct without having to track every penny individually. All we have to do is look at the inflows and outflows and check that they balance. And we can do exactly the same with waiting lists. It looks like this:
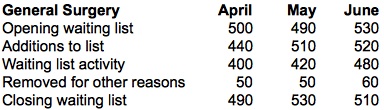
If you do those accounts with the raw data for a typical hospital waiting list, the numbers do not balance. In my experience they are typically out by something like 10 per cent. You wouldn’t tolerate that on your bank statement, and now we need to take the same attitude to our waiting list data. So the first thing you need to do is put somebody in charge of these waiting list “accounts”, somebody for whom any imbalance strikes against their very soul. This is a job for an accountant.
In fact, you’re going to need a lot of the paraphernalia of accountancy: waiting list “accounts” at service level; aggregate accounts at specialty, care group, and Trust level; and auditing systems. But most of all you need to develop a culture that these “accounts” must balance everywhere at all times because, if they are out by just one patient, then that is a patient who might fail to receive the care they need and is therefore at risk.
Commissioners: this involves you too. You may not be covered by the criminal offence (which applies only to care providers) but these are your patients and you need to be sure they are being looked after. So take an interest, work constructively with providers, and write into the contract that they must share with you their detailed waiting list “accounts”. You already make sure the money you send them balances, and it is even more important to do the same with patients.
Yes, this is going to be a lot of work, especially at first. But it’ll be worth it. Here is an opportunity to break the cycle of inspection and punishment, and deliver a valuable goal that has no down-side. The time to start is right now. Then, when the Bill is passed and the offences come into force, Plod and all the inspectors can whistle because you’ve already sorted it out.
And, best of all, you won’t feel anxious every time you see a police car parked outside the hospital.
—————-
