
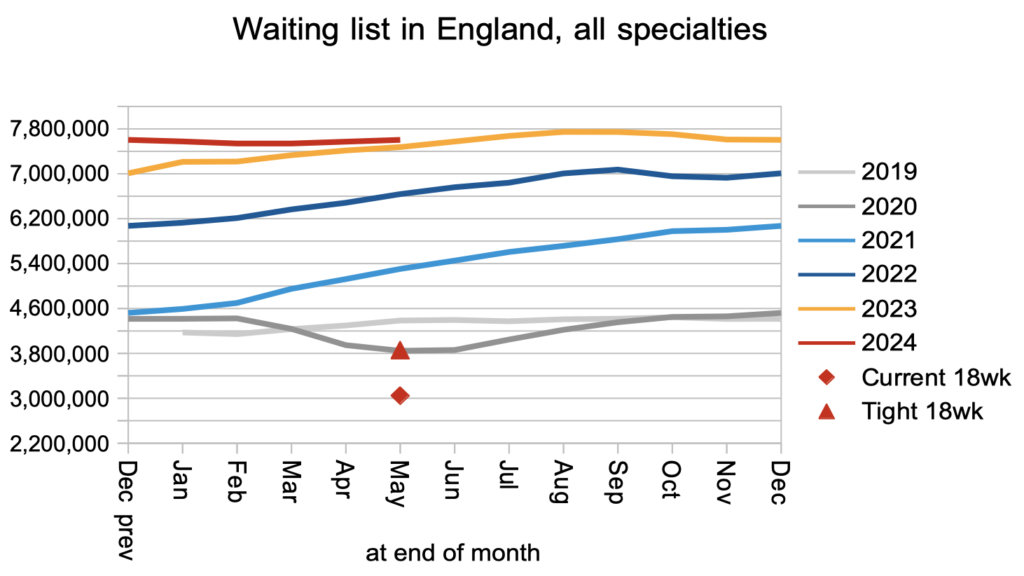
The waiting list grew by 31,000 patient pathways in May, bringing the English referral-to-treatment (RTT) list size to 7.60 million. May was the penultimate complete month of the last Conservative government, so this increase counts against the former prime minister’s pledge that the waiting list would fall.
Analysis produced for Health Service Journal by Dr Rob Findlay, Director of Strategic Solutions at Insource Ltd and founder of Gooroo Ltd
The number of over 65 week waiters rose by 5,600 to 56,000. The target – set under the Conservatives – is to eliminate 65 week waits by September. The typical RTT waiting time rose slightly by 0.2 weeks to 44.95 weeks, and the incoming Labour government has pledged to reduce this to 18 weeks by 2029.
In the following discussion, all figures come from NHS England, and do not yet include the data revisions since October 2023 which were released simultaneously. You can look up your trust and its prospects for achieving the current waiting time targets here.
The numbers
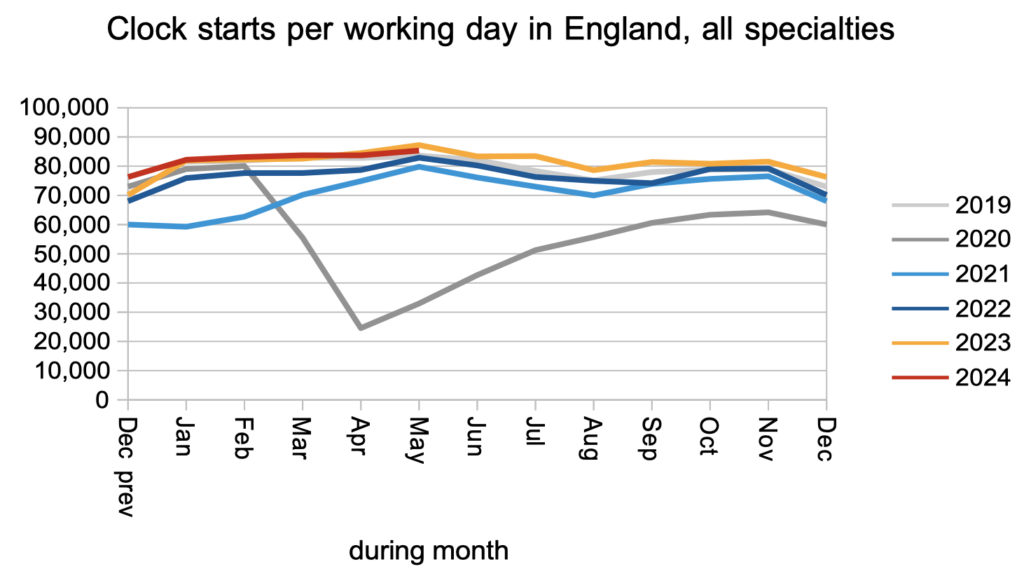
Demand remained at pre-pandemic levels, as measured by the number of patients starting new waiting time ‘clocks’.
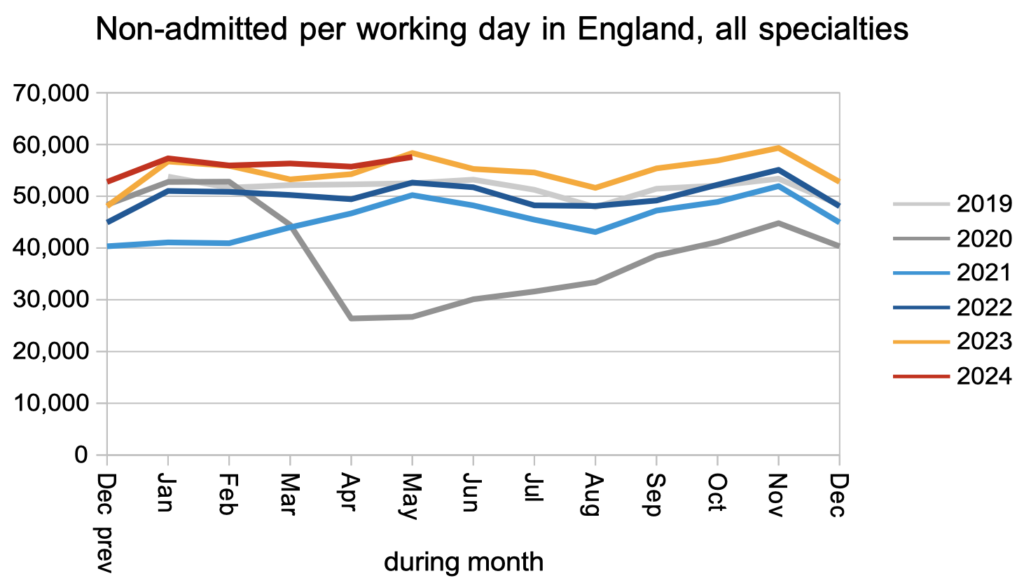
Patients were discharged from the waiting list at the outpatient and diagnostic stages of the pathway at higher than pre-pandemic rates, and broadly the same rate as this time last year.
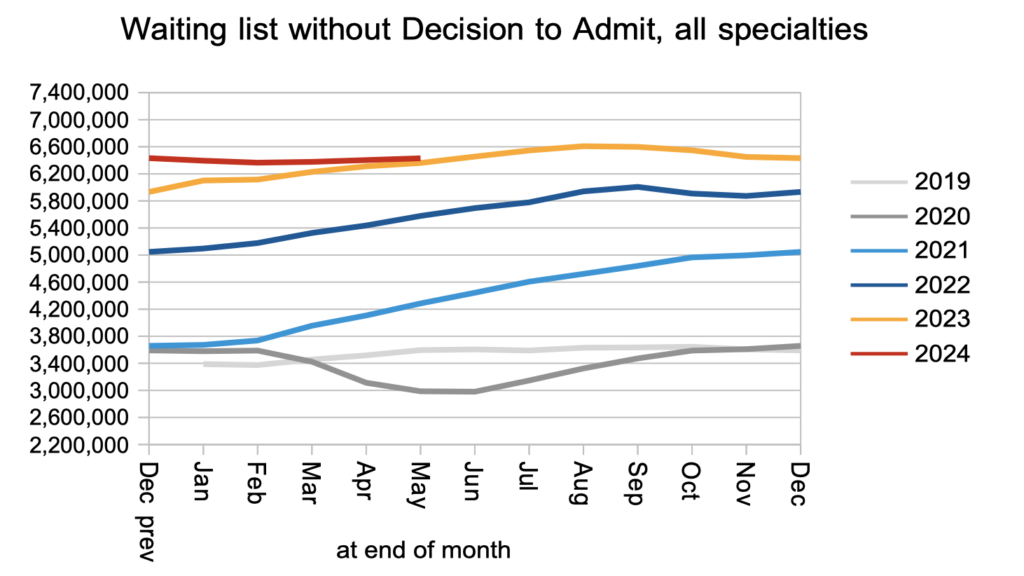
The net result of those clock starts and non-admitted clock stops, together with those who moved on from this stage of the waiting list following a decision to admit, was that the waiting list for outpatients and diagnostics remained roughly steady. In amongst them are an estimated 27,834 patients whose eventual diagnosis will unexpectedly be cancer. They are not protected by the cancer waiting time targets because their cancer is not yet suspected, so they will wait as long as everyone else for a diagnosis and decision: typically 42.7 weeks, which is far too long when that diagnosis is cancer. The only way to tackle this clinical risk is to reduce the waiting time to diagnosis and decision for all patients.
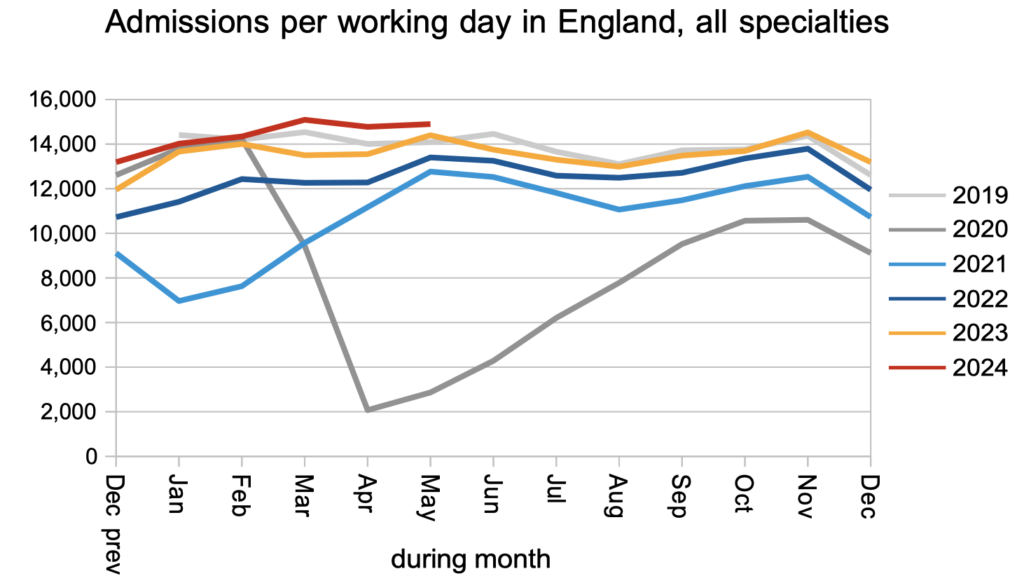
Patients were admitted for inpatient and daycase treatment at above pre-pandemic rates, and faster than last year.
The net result of all those clock starts and clock stops, together with administrative removals from the list (and significant data quality problems), was that the reported waiting list grew slightly. This is not as bad as it might seem, because the waiting list usually grows seasonally at this time of year even when the NHS is broadly keeping up with elective demand.
Waiting times grew slightly in May, to 44.95 weeks RTT, on the statutory ’92 per cent of incomplete pathways’ basis. The incoming Labour government has pledged to restore this to 18 weeks during their first parliament (i.e. by 2029). As mentioned above, the waiting time to diagnosis and decision to admit rose to 42.7 weeks.
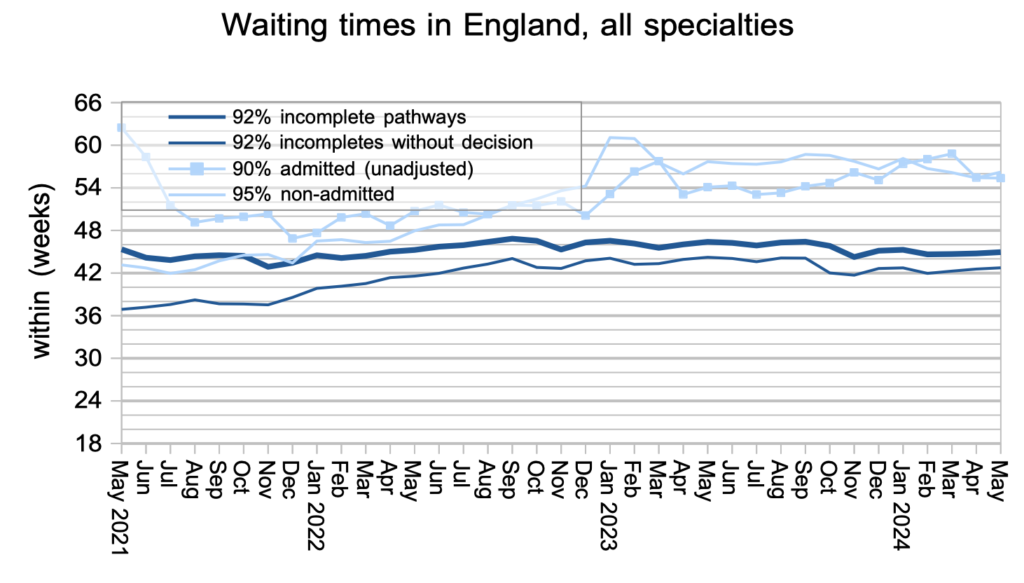
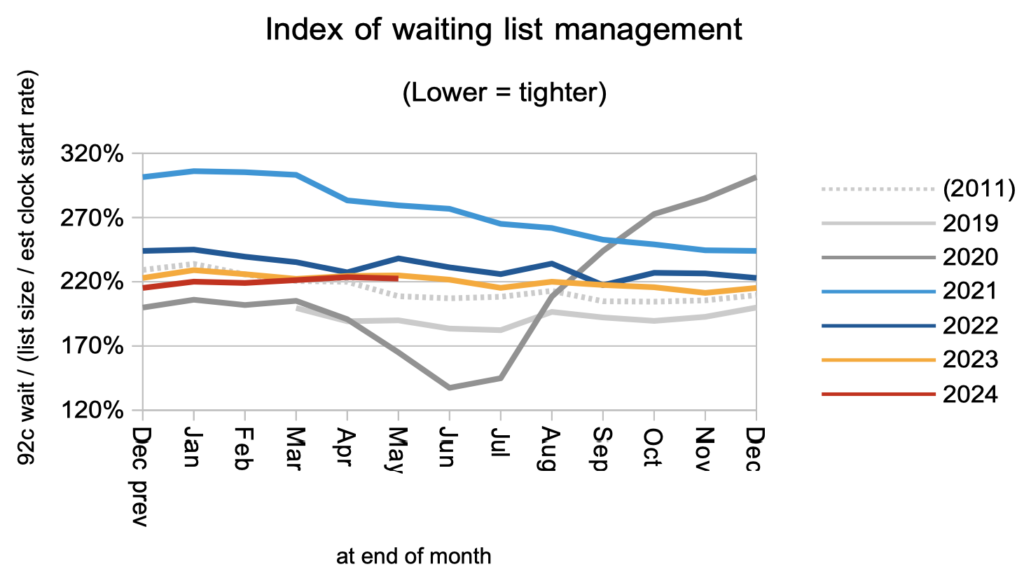
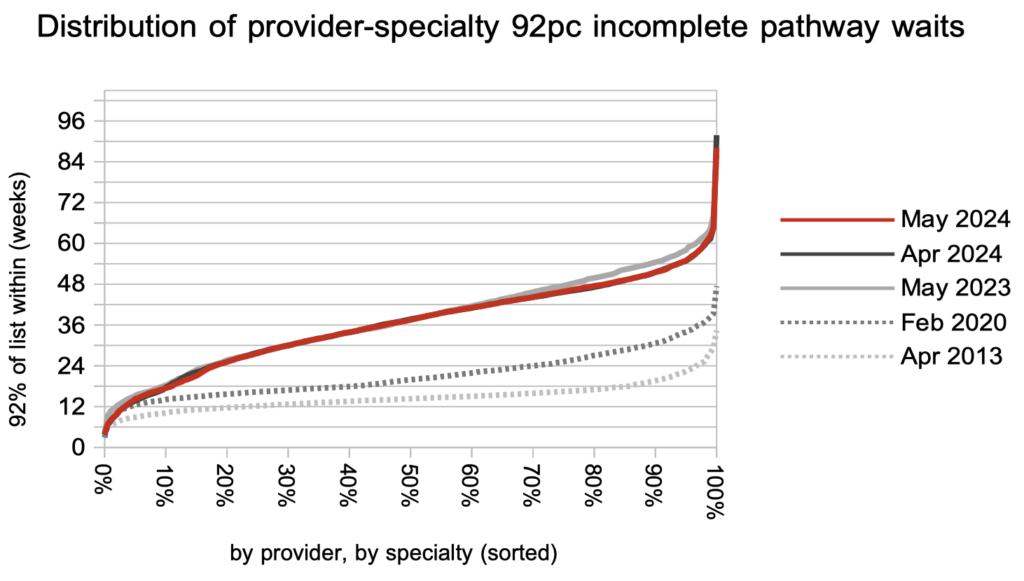
Waiting times are a function of both the size and shape of the waiting list, and the shape does vary considerably. It worsened (became longer-tailed) during the pandemic and remains significantly worse than it was between 2013-16. The red triangle and diamond in the waiting list size chart above show how big a difference the waiting list shape makes to the difficulty of restoring the 18 week standard.
ENT remained the longest-waiting specialty at national level. Ignore the mental health waiting times in the chart below, because the apparent improvement is an artefact of a large trust dropping out of the data series.
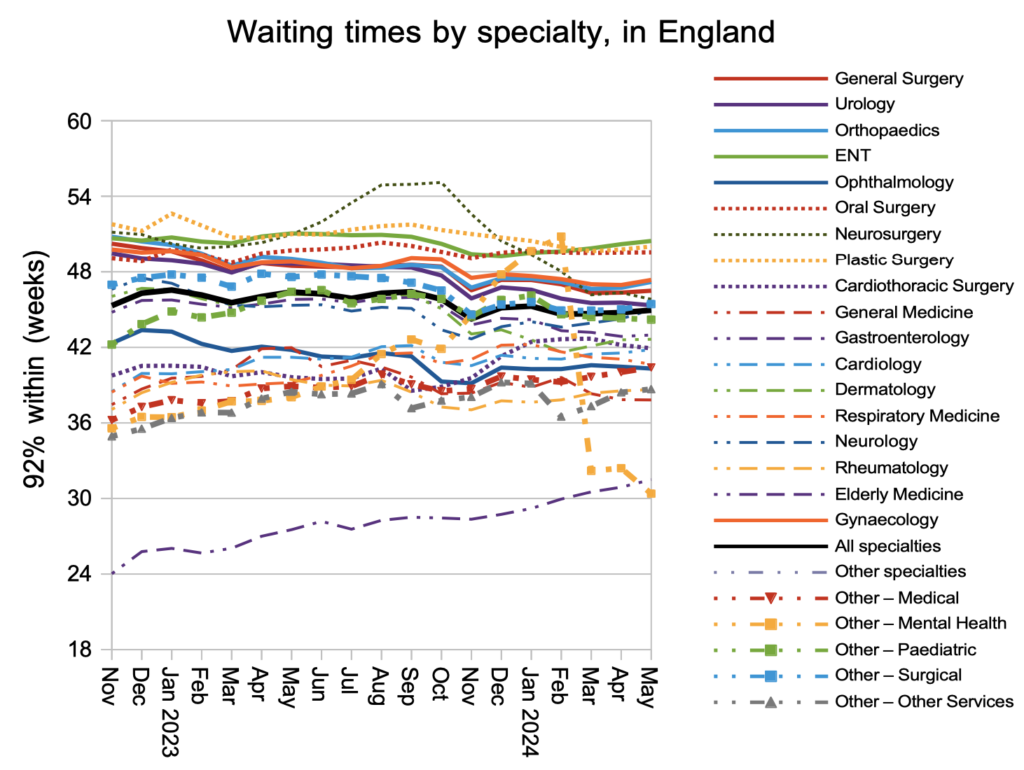
Over the past year, the longest waiting times have generally improved in response to the targets, while the waiting time experience for most patients has not changed.
Referral-to-treatment data up to the end of June, which is effectively the closing position for the last Conservative government, is due out at 9:30am on Thursday 8th August.
