NHS Highland NTC opens to fast-track Ophthalmology and Orthopaedic waiting lists. And unified data and informed patient selection are central to its success. This powerful POC forms the foundation of a ‘Once for Scotland’ potential implementation across all NTCs.
With the National Treatment Centre Highland opening this week the key priority is to tackle ophthalmology and orthopaedic patients and ease the suffering of more people fast. But with such huge backlogs the health board must guarantee that not only are they optimising the waiting lists and treating patients fairly, by length of wait and clinical priority, but are also maximising theatre time to ensure more patients can be treated overall. A key aim of the centre is to keep all theatres and clinics full.
The NTCs in Scotland are the equivalent of Surgical Hubs in England and with help from Insource, unified data from disparate systems across the area and informed patient selection are central to its success.
NTC Highland

The National Treatment Centre in NHS Highland is a purpose-built Centre for both surgical and outpatient eye care services, uncomplicated hip and knee replacements, and foot, ankle, and hand day-case surgery. It encompasses 13 consultation rooms, 5 theatres and 24 beds and is part of 10 NTCs funded by the Sottish Government. It draws waiting list patients largely from NHS Highland but also handles referrals from NHS Grampian. The Scottish Government have agreed a Target Operating Model with the NTCH of delivering 4 joints per day, 16 cataracts per day, zero on the day cancellations, no under and over runs in theatre with a tolerance of 5% and a 95% theatre utilisation rate by Year 2.
To ensure the NTC fulfils its primary objective, to reduce the waiting lists, and to ensure money from the public purse is well spent, Highland are working hard to ensure the NTC is working at maximum capacity and the following successful POC detailed below is part of a ground-breaking project.
Key challenges
Despite the backlogs, surgeons are still spending very little time on ‘knife to skin’ procedures. Some NHS Highland consultants estimate this is as little as 15% of their total week. All surgeons want to do more but are often plagued with excessive administration, cancellations on the day of surgery and wasted theatre slots. Whilst DNAs are a major issue, inadequate access to minimum / maximum / average procedure timings when scheduling theatre staff and equipment also has a big impact. Under-runs in theatres are inefficient and over-runs are putting huge strains on staff welfare when they need to get home for families. Lack of a clear picture of anticipated length of stay and projected bed availability are also severely limiting factors.
Getting the complete picture for streamlined surgical care
In order to get the right patients to the NTC, at the right time, staff need the complete picture. Accurate data that is retrieved from numerous disparate systems across the care landscape from TrakCare PMS, SCI Gateway, TheatreMan, diagnostics, care contacts, +++ and combined into a single version of the truth, a Unified Data Layer – is vital. This single source of fully validated data enables operational teams and clinicians to see the full patient journey to date before scheduling them into the NTC.
Patient selection is key if the NTC is to operate at maximum capacity and deliver safe patient care. To be useful this data needs to include:
- Up to date patient demographics including how far they are from the centre to ascertain if they could come in quickly if a slot becomes available at short notice and to determine what time of day they can be scheduled to ensure they can return home same day without the need for an overnight stay
- Length of wait and clinical priority
- OPCS codes/site code
- The patient’s anaesthetic fitness (ASA score)
- Theatre equipment availability
- Anticipated length of stay
- Critical care requirements
- Min/max/average procedure time
- Laterality
With this data to hand and populated automatically the NTC can then plan theatre timings, length of stay or day-case, bed occupancy levels, and post-operative care and hand-off. Then patient communications can be initiated to schedule them in and start the process of pre-operative assessment.
Unified data the basis for effective scheduling
Previously the administrative process to book patients in was very manual and paper based, and many concerns had been raised by staff on this. With the Insource elective recovery suite all this data will be available digitally for fast patient identification and scheduling. Below is a diagram which depicts the complex high-level workflow of a patient who has been assessed as suitable for admission to the NTC through to the patient receiving their procedure.
Essential information is required from numerous disparate systems. The Insource solution brings all required and relevant data together, standardises and DQ checks it and presents it into the Unified Data Layer so that everyone involved in the process has access to the same and latest information.
Only with the information unified in one place can an accurate assessment of patients be made to ensure that patients are chosen in the right order according to time on the waiting list and clinical priority, and that the correct patients are then chosen in the right order to ensure the most efficient utilisation of theatre time. The sheer number of different systems on which the necessary information is held means that it would be impossible to manage a fully inclusive and accurate PTL if the information wasn’t brought together to be presented as a single entity.

The POC at NHS Highland was to create the first step in this process and the first electronic pre-operative ‘Picking Lists’ have already been developed and are now in use at NHS Highland using the Insource Solution:


They comprise:
- Pre-operative assessment picking list – in date order
- Booking list for patients technically suitable for NTCH with ASA 1 & 2 scores
- Availability for surgery with distance to travel
- Consent clinic list – for patients who have been provided a provisional date for surgery
“This is ‘revolutionary‘! I created my theatre list for the month in half an hour, it usually takes that long per theatre list.”
Colin McNair, Clinical Director, NHS Highland
Maximising theatre and bed capacity
With this data-rich foundation, tight scheduling can maximise theatre usage and surgeon operating time. The targets agreed by NTCH include delivering 4 joints per day, 4.5 foot and ankle, 4 hand surgery patients per day, 16 cataracts, zero on-the-day cancellations, no under- and over-runs with a tolerance of 5%, and a 95% theatre utilisation by Year 2.
Whilst this may seem a tall order, It is proposed that while a Theatre utilisation tool such as Infix (or any similar solution) will choose patients to ensure ultimate efficiency of theatre time regarding demand and capacity, Insource can ensure that the patients are chosen in line with clinical priority and the legal Treatment Time Guarantee ensuring that no patients wait longer than necessary, are chosen out of turn or get lost in the system – And ultimately that no patients come to harm while waiting for treatment.
Theatre scheduling and staff database interface
Infix is a clinically led, cloud enabled technology platform targeting significant improvements in theatre efficiency. It holds 5 year’s data related to NHS operating times that can be used to allocate slots and drive efficiencies in theatre planning and scheduling. It is deployed in numerous NHS sites in Scotland and has demonstrated 26.8% efficiency gains.
Infix matches accurate operating times specific to ISD codes to maximise allotted slots to available time. The solution interfaces with the existing staff database to ensure operating lists are matched to the correct skill sets and staff availability. And the at-a-glance KPI dashboard and real-time analytics allow performance measurement throughout and a proactive response to changing waiting list demands. However, the Infix solution is only one piece of the jigsaw which makes up the complete picture of the elective care solution. There would be little point in choosing patients to utilise theatre time if the patients were not being managed in line with the legal requirements of TTG. Infix or similar theatre scheduling solutions can easily be integrated into the overall elective care solution.
NHS Highland booking process
Highland is introducing a 6, 4, 2-week theatre booking process in line with best practice. Theatre lists will be reviewed on a weekly basis to ensure surgeons/anaesthetic/theatre staff are available 6 weeks out. Patients are booked 4 weeks out and the lists is locked down 2 weeks out. The rules of engagement are that at 2 weeks out any cancellations will be replaced with a patient waiting for the same procedure with the same anticipated length of stay. Beds will be booked at the same time as theatres to prevent cancellations due to lack of beds.
Reducing waiting times and delivering best practice
NTCH has demonstrated that, moving from 4 to 5 patients per day for Fasciectomy hand surgery, will reduce the time to deliver 12-week waits in that specialty by 5 years. They aim to reach zero on-the-day cancellations with improved patient instructions, guaranteed equipment and staff availability, and fast turn-round of patients to fill short-notice slots. They are also looking to avoid multiple pre-operative assessments (POAs) by booking patients at the time of assessment against theatre and bed availability. And the aim is to increase zero-day length of stay for primary joint replacement with improved list management to support the pre-rehabilitation work with patients.
This informed, integrated solution allows the workforce to be agile and responsive to emergent demands. And the consistent use of operation codes, benchmark times and comparable reporting metrics enable NTCH to share best practice and above all create a fast reduction in the backlogs.
Benefits
- Patient Harm is significantly reduced – Waiting times are reduced, no patients lost in the system or overlooked
- Everyone is working from the ‘Single Version of The Truth’
- Proactive management of waiting lists allows for visibility of patients due to breach within x weeks so breach can be avoided
- Need for overnight stays reduced as patients can be booked in in order of how far from the NTC they live – those living further away can be booked in earlier in the day
- Volumes of patients flowing through NTC’s increases
- Positively impact the number of DNA’s
- No more overruns of Theatres allows better work-life balance for staff
- TTG & NTC waiting times by BoR and BoT
- NTC performance monitoring unlocked
- Complete visibility and near real time access to “locate” any patient and see stage within any NTC by each Health Board
- Visualise & analyse theatre efficiency, extract dashboards, e.g., Heatmaps of activity.
- Enable allocation of capacity through visibility of demand & activity
- See where the bottlenecks are and uncover hidden capacity
- Reduction in patient cancellations as a result of no bed by utilising data on expected length of stay with bed availability
- Reduction on the day cancellations with an improved / reliable Special Instructions – to make the right equipment / components available in Theatre
- Increase Zero Day Length of stay for Primary Joint Replacement with improved list management to support the pre-rehabilitation work with patients
- Reduction in multiple Pre-Operative Assessments by booking patients at POA to match capacity that is available in the NTC
- Availability of Data Quality reports to ensure compliance with SOPs, to improve the patient experience and move to providing the date for surgery at the consenting clinic.
- Share best practice more seamlessly nationally through consistent use of operation codes, benchmark times and comparable reporting metrics
- Creation of a national performance dashboard that provides a snapshot of live data
- Automated reporting
- Improved theatre utilisation to support the delivery of 95% theatre utilisation by Year 2 of opening within the NTC.
- Reduce time and pressure on administration staff and enhance their roles
- Reduce paper and manual processes and improve the ability for staff to work remotely
Conclusion
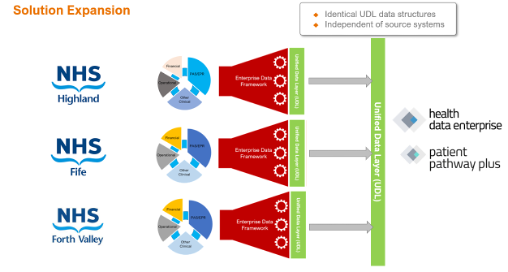
While the Insource Solution is the Solution of choice for NTC Highland and the recent Proof of Concept utilising this solution to produce an accurate and robust electronic picking list proved the solution meets the complex requirement of having all disparate data brought together electronically into a Unified Data Layer, the solution is fully scalable. The solution allows for patients to be treated at alternative NTC’s, as Patient lists and reporting can be managed at both Board of Residence and Board of Treatment. The Insource fully scalable solution can provide a Unified Data Layer across several Health Boards, as in the diagram below, and can be scaled for a Once for Scotland solution for the National Treatment Centres and for the delivery of elective care across all Health Boardss.
While this paper reports on the progress and solution for NTC’s, there is no reason why this same solution couldn’t be used for managing TTG or Cancer waiting lists across individual, multiple or Once for Scotland Health Boards. Indeed NHS Highland have realised many benefits and are successfully using this Insource Solution for managing their Cancer Patient Waiting Lists.