Today [17th November 2011] in the HSJ, Anthony McKeever and I make the case for an upper limit on waiting times in England: a guaranteed one-year maximum waiting time from referral to treatment, that no patient should ever be made to breach.
But is it possible? At first glance it looks easy. The NHS in England treats and discharges over a million patients from the waiting list every month. There are fewer than 20,000 patients waiting more than a year. So that’s equivalent to less than 3 hours’ work. Even if we assume that all 20,000 need to be admitted (and could not be treated in or discharged from outpatients), it’s still less than 12 hours’ worth of admissions.
So all we have to do is take some of the routine patients who we currently treat much sooner, make them wait a couple of days longer, and spend those two days clearing the over-one-year waiters. Easy. Let’s start tomorrow.
If only life were so simple. There are clinical priorities to take into account – and the over-one-year waiters are not spread evenly across the NHS. Around 40 per cent of Trusts have none at all, so they would be twiddling their thumbs during the two “clearance days”. Six Trusts (we are using the August 2011 figures for England throughout this post) have over 1,000 over-one-year waiters, which would keep them busy for longer than two days. This interactive map shows where all the over-one-year waiters are:
Long-waiters are clustered by specialty, as well as by Trust. This is an even bigger barrier than geography, because gynaecologists cannot just scrub up and do a couple of orthopaedic lists. Although patients can easily be offered the choice of quicker treatment at another hospital, they cannot be offered treatment by another specialty.
This clustering by specialty and Trust means that, if we want to understand how we could achieve a one-year maximum wait, we need to go right down to Trust and specialty level. (A local analysis would go further, to consultant level, but for now we are restricted by the published RTT data which only goes down to specialty.)
Treating the one-year-waiters
At Trust and specialty level, if we divide the number of over-one-year waiters by the rate that patients are admitted, we can calculate the number of working days it would take to clear the one-year waiters: the so-called “clearance time”. (We are erring on the side of caution by assuming that all these patients need to be admitted; in practice many will prove on validation to be miscoded, or can be treated and discharged from outpatients.)
There are 169 Trusts in the data we are looking at, with an average of nearly 8 waiting list specialties in each Trust: 1,331 Trust-specialty combinations in all. So here is the distribution of clearance times for all 1,331 Trust-specialties in England:
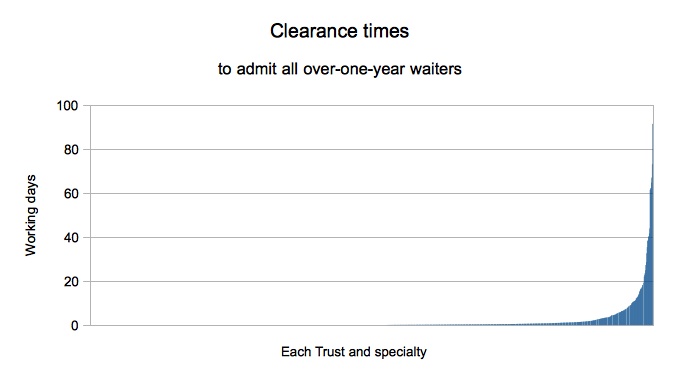
The over-one-year waiters are highly concentrated: only 87 Trust-specialties have clearance times over a week (5 working days), 49 over 2 weeks, and just 21 over 4 weeks.
Those Trusts will have neighbours who could take on some of the work. Most patients who have already exercised Choice (and met their consultant, waited for ages, and are now expecting to be treated soon), might not choose to switch provider. But capacity can equally be freed-up by extending opportunities for newly-referred patients, so they can choose an alternative provider where patients are not kept waiting for a year. This could be done through the existing Choice mechanism, and this could be facilitated using national-level expertise to ensure that Choice is extended in a targeted manner around each highly-pressured service.
On the basis of these numbers, then, there are just a few dozen Trust-specialty hotspots that need really close attention; not an insuperable task on a national scale. This is looking promising.
Improving patient scheduling
But there are problems with trying to clear one-year-waiters simply by treating them. Back in the 1990s, “waiting list initiatives” were commonly used all over the country in an effort to “chop the tail off” the waiting list. Unfortunately, the tail tended to grow back again, usually within a few months. Behind the 12-month waiters stands a cohort of 11-month waiters, and behind them stands an even larger cohort of 10-month waiters, and every month they all shuffle forward. So what can we do?
We know that waiting times can be reduced with better patient scheduling. Our daily experience of queues tells us that if some people queue-jump then other people wait longer. In our daily lives, fair queues are first-come-first-served. In healthcare things are more complicated because we have patients with cancer and other urgent conditions, and they quite rightly need to jump the queue on routine patients. So the four principles of good NHS waiting list management are:
1. Higher clinical urgency means shorter wait.
2. Similar clinical urgency means treat (broadly) in order of arrival.
3. Keep the longest waits down to a reasonable level.
4. Do all this without impairing the efficient use of capacity.
When Trusts have waiting time pressures on the scale we are discussing here, they may feel that the standard NHS contract inhibits their scope for treating long-wait patients. The contract allows commissioners to apply financial penalties to Trusts if they admit a high proportion of over-18-week waiters, which can limit Trusts’ ability to tackle long-wait backlogs. The corresponding waiting time measures that are monitored and promoted nationally could have a similar effect.
It would be helpful if it could be agreed that these penalties and measures should not be applied to those Trusts and specialties with the longest waiting times, in return for allowing them to tackle their backlogs wholeheartedly and achieve sustainable one year maximum waiting times. In the next bit of analysis we shall assume that an ‘amnesty’ is put in place for a while.
We are going to estimate the maximum waiting times that each Trust-specialty could achieve, if it managed its waiting lists according to the four principles above. There are, of course, quite a lot of assumptions behind these calculations, and you’ll find them in the footnote*. Here is the distribution:
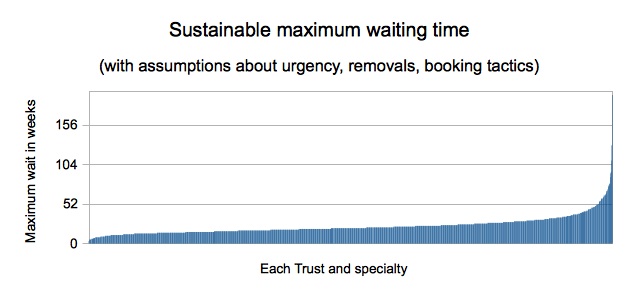
According to these estimates, all but 34 Trust-specialties should be able to achieve maximum waits below one year by applying the disciplines that underpin best practice. This is a smarter solution than brute-force waiting list initiatives, because better patient scheduling improves maximum waiting times in a sustainable way. The “tail” doesn’t “grow back”.
Improving scheduling is not a trivial task, but there is scope for sharing experience and expertise to help Trusts work through the issues and processes involved., Many Trusts have found it challenging to implement Choose and Book in ways that are consistent with the principles of good waiting list management. But that’s not to say it can’t be done – there is just a need to reinforce success and to spread learning. Internal mechanisms like the IST and IMAS have a good track record in supporting places that struggle.
But no amount of good waiting list management can stop waiting times from going up if the backlog is growing relentlessly. So services with severe waiting time pressures need to agree future plans with their commissioners that ensure the waiting list will shrink rather than grow. Pressures vary from place to place, of course, but nationally the waiting list is not currently rising year-on-year so we are not in the position of fighting a relentlessly incoming tide.
If those ingredients can be put in place then one-year maximum waiting times are starting to look very achievable.
Better scheduling plus backlog clearance
Ideally we want to combine both approaches: better scheduling, and one-year backlog clearance. The next chart makes a start at putting these two approaches together.
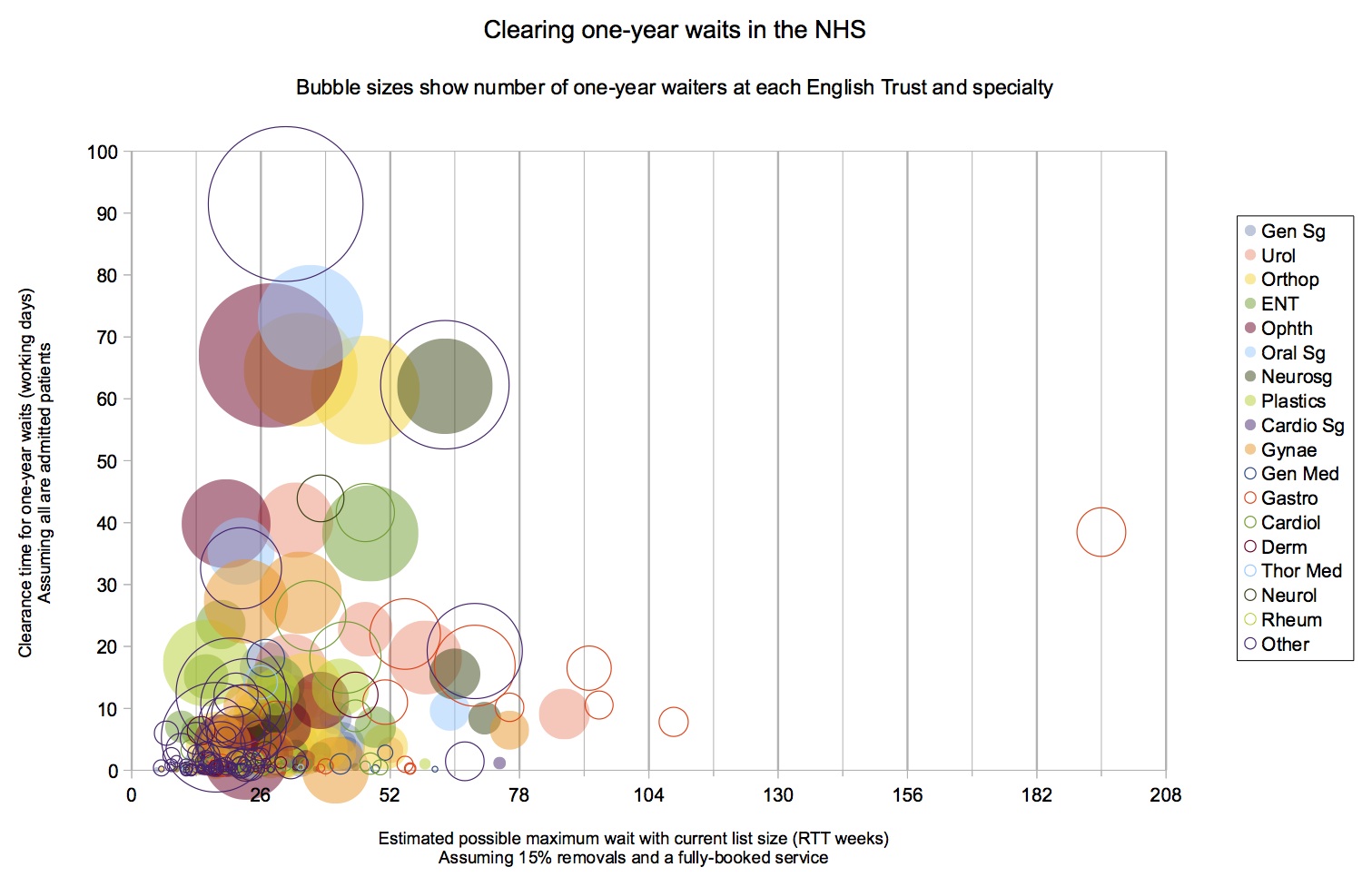
Each “bubble” represents a single specialty at a single Trust. The size of the bubble shows the number of over-one-year waiters. Its position on the horizontal axis shows the sustainable maximum waiting time (without any backlog clearance). Its position on the vertical axis shows the clearance time for admitting all the over-one-year waiters (without improving scheduling). Different specialties are plotted in different colours, with surgical specialties as discs and medical specialties as circles.
The first thing to notice is that most Trust-specialties with over-one-year waits could at least halve their maximum waiting times, if they improved their patient scheduling practices in line with the principles of good NHS waiting list management; most of the bubbles on the chart are to the left of the 26-week line.
Looking at the services with the greatest pressures, we can see that many of our biggest challenges in terms of backlog clearance (towards the top of the chart) could probably achieve a one-year maximum wait with better scheduling alone (the centre of their bubbles lie to the left of the 52-week line). Conversely, many services with high achievable waiting times (to the right of the chart) have relatively short clearance times (they are close to the bottom). This is excellent news, as it suggests there are relatively few services that could not be brought within a year with a combination of methods.
In fact there are only 11 Trust-specialties with one-year clearance times over 10 days and sustainable maximum waiting times over 1 year. The table below shows these 11 services. For each one, we have calculated the effect of applying both better scheduling and backlog clearance together: we worked out the size of waiting list needed to sustain a one-year maximum wait, and then worked out the clearance time needed to achieve that list size, on the (cautious) assumption that all patients need to be admitted. (In some cases, the reduction in list size is larger than just clearing the over-one-year waiters.) Here are the results:
| Specialty | Trust | Clearance time to one-year sustainable max wait (working days) |
| Gastroenterology | Wirral University Teaching Hospital NHS Foundation Trust |
890 |
| Gastroenterology | Croydon Health Services NHS Trust |
220 |
| Gastroenterology | Royal United Hospital Bath NHS Trust |
162 |
| Gastroenterology | East Sussex Healthcare NHS Trust |
143 |
| Other specialties | Wirral University Teaching Hospital NHS Foundation Trust |
112 |
| Neurosurgery | The Newcastle Upon Tyne Hospitals NHS Foundation Trust |
71 |
| Other specialties | St George’s Healthcare NHS Trust |
55 |
| Neurosurgery | St George’s Healthcare NHS Trust |
44 |
| Urology | United Lincolnshire Hospitals NHS Trust |
27 |
| Gastroenterology | St George’s Healthcare NHS Trust |
21 |
| Gastroenterology | Guy’s and St Thomas’ NHS Foundation Trust |
12 |
Surprisingly, no orthopaedic services make it onto the list. Of the 11 Trust-specialties that do, a majority (6) are in gastroenterology (a high-urgency specialty with many planned patients, some of whom might be miscoded), 2 in neurosurgery (which is only provided in a few Trusts), 2 in “other specialties” (the nature of which will vary from Trust to Trust), and the remaining one is urology. All of these would need to be looked at closely and locally to validate the list, establish the true level of clinical urgency and other service issues, and develop plans to ensure that the waiting list will shrink rather than grow in the future.
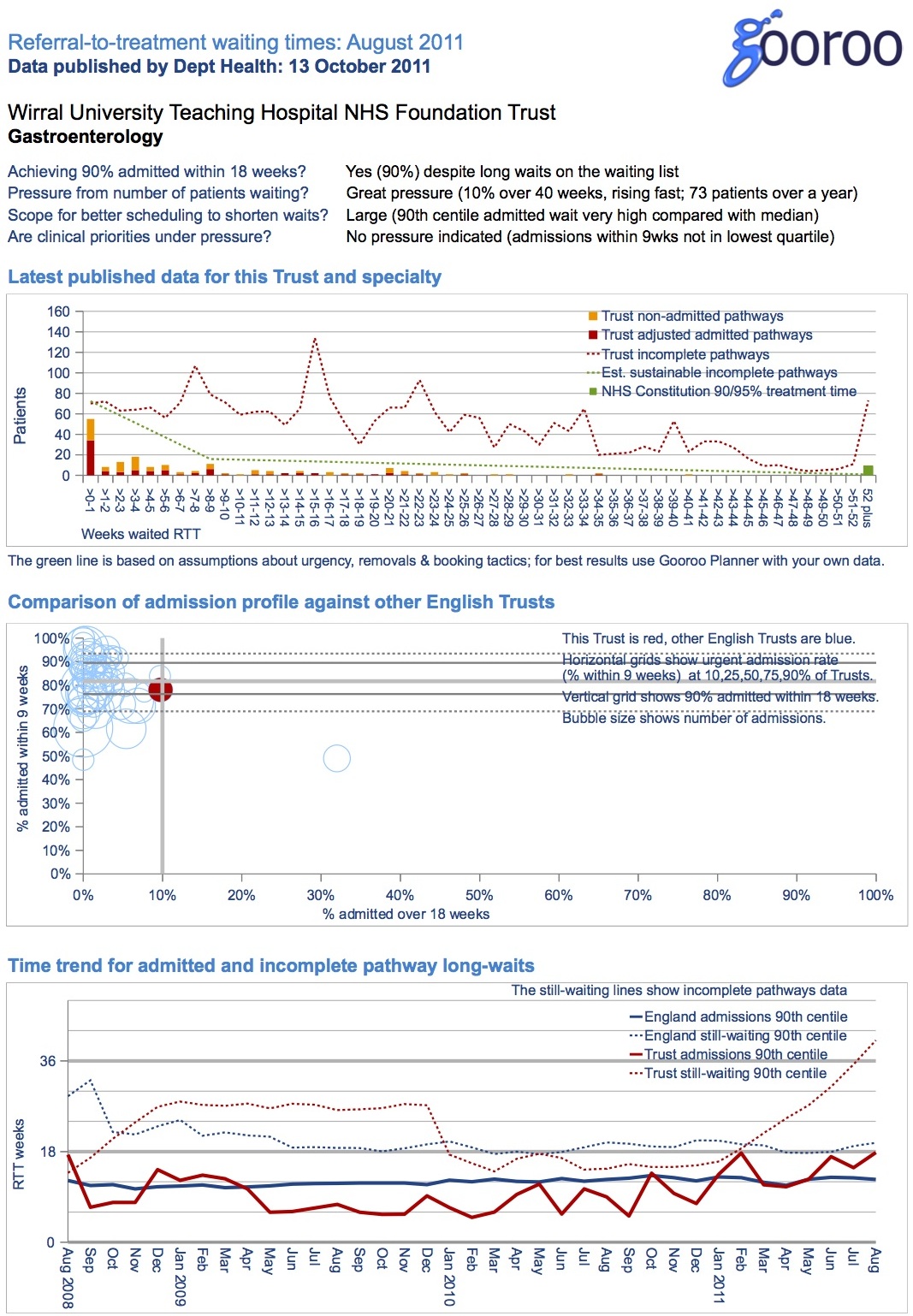
Looking at the table above, you are probably curious about the extraordinary result at the top of the table for Gastroenterology at the Wirral. Here is the detailed analysis (and similar reports are available for all Trusts and specialties at www.gooroo.co.uk/reports). This is a striking example of a service achieving the NHS Constitution target that 90 per cent should be admitted within 18 weeks, even though as many as one in ten waiting list patients are breaching 40 weeks.
Conclusion
The big question is: could the NHS achieve a one-year maximum RTT waiting time? Our analysis points to a resounding “yes”. Would it cost a lot? No, perhaps no more than the administrative costs of a national initiative.
The reason, in a nutshell, is that very few Trusts and specialties have severe one-year waiting time pressures, and there is scope for using Choice in targeted ways to divert patients to other Trusts that have the capacity to meet both their clinical needs and their reasonable expectations in terms of waiting times. There is also considerable scope, if certain existing contractual and managerial measures can be waived, to make waiting times fairer and shorter by improving patient scheduling.
The Infrastructure required to support a national drive on one-year waiting times is, we believe, already in place at national level and could be focused temporarily on the task for the six months or so it would take to complete. We expect that DH and the NHS Commissioning Board could support health economies in a number of ways:
> by asking Commissioners to pinpoint Trust-specialties that have the greatest pressures and to agree recovery plans for dealing with them.
> by rewarding GPs that take positive action to eliminate excessive patient waits as part of the authorisation process for their Clinical Commissioning Groups;
> by exploring ways of developing a “clearing house” to match backlogs with available capacity elsewhere;
> by providing operational expertise to help Trusts optimise their patient scheduling (including through Choose and Book);
> by ensuring that other aspects of contract and performance management do not inadvertently impede progress; and
> by insisting that high-pressure services are planned so that waiting times will continue to remain below one year.
In today’s HSJ article we explained why a maximum one-year wait is worth achieving. Here we have shown that, with a deliberate effort, it can be achieved. And we hope that, before very long, it will.