“Cancellations push up waiting times. So does a big waiting list. Common sense, isn’t it? You don’t need a model to tell you that.”
All true. But what common sense doesn’t tell you is how much they push up waiting times. This matters when you’re looking at a 10-week outpatient wait and trying to get it down to 8 weeks – you need to know how big an effort you’re going to need.
So what does increase waiting times? And is there anything you can do about it? If you can answer those questions, then you’re well on the way to cutting waits at almost no cost, and without wasting valuable time trying to fix things that don’t actually matter.
This post reports on simulation research by Gooroo that investigates the (sometimes surprising) effects of different kinds of disruption on waiting times. (It does not consider the effects of good and bad practice when booking patients; that will be left for a later post.)
Things that make a big difference
Urgency of casemix
Urgent patients, by definition, need to jump the queue because of their clinical conditions. And the more queue-jumping there is, the longer other patients wait, and the longer the longest waiting times.
Similarly, just how quickly these “urgent” patients need to come in also makes a significant difference to waiting times. The quicker they come in, the more other patients are pushed back, and the more the longest waits go up.
All this is well-established, and the routine waiting time you would expect as a result can easily be calculated.
But something else happens as well. Urgent patients also cause a lot of general disruption when booking patients. The more urgent patients there are, the more disruption there is. Both the number of longwaits (after taking into account the queue-jumping effect), and other undesirable events (like delayed urgent patients and rebooked routine patients), increase steadily as the urgency of the casemix goes up.
You can’t alter the clinical urgency of the patient. But you can increase the care taken to describe their clinical urgency accurately. If urgency is being systematically over-declared, then waiting times are being needlessly increased. So it is worth paying close attention to the process and criteria used to declare the urgency of patients.
Number of patients waiting
If a list gets bigger (relative to activity) then waiting times go up. Again this is well-known, easily quantified, and the expected routine waiting time can be calculated with the size of the waiting list taken into account.
But again, there are additional effects. Bigger lists suffer much more disruption than smaller ones. Again the disruption increases the number of longwaits who exceed the expected routine waiting time, though it does not greatly affect urgent patients or rebookings.
Controlling the size of the waiting list is already a priority throughout the NHS, so this finding merely adds emphasis.
Removals
Here “removals” means those patients who are removed from the waiting list well before they come in for their appointments. If a patient already has an appointment booked, then this is cancelled and reused for another patient.
You might expect removals to cause some disruption, but not much. But that expectation does not account for the sheer numbers of patients removed from NHS waiting lists. For admitted patients (inpatients and daycases) it is quite typical for 15% of patients to be removed, and often as many as 25%. At such high volumes of removals, the level of disruption is huge, with longwaits and rebookings being the main consequence.
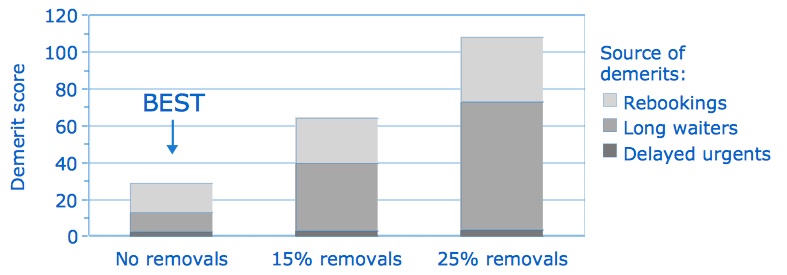
So any action that might reduce the number of removals, by ensuring that patients are only added to the waiting list if they are likely to proceed with their appointments, would be beneficial.
(Suspending patients is not currently practised in England, but is used elsewhere, and this practice has a smaller effect on longwaits and rebookings.)
Modest effects, but still worth looking at
The following effects would be worth looking at too, but more for reasons other than reducing disruption.
If patients are cancelled on the day of their appointment and subsequently rebooked, this causes a moderate increase in disruption, in addition to the waste of capacity caused by their unused appointment slot. (Patients who are cancelled but not rebooked, like many Did Not Attend (DNA) patients, waste capacity but do not cause disruption.) If the main motivation for tackling cancellations is to reduce wasted capacity, then deliberately over-booking every session (and accommodating the resulting variability in session length) would be worth considering as a compensating tactic.
If significant numbers of patients are pooled between several clinicians, this helps to even out waiting times (and therefore reduce the maximum waiting time for the service). This levelling of waiting times should be the main motivation for this tactic. As a useful side-effect, it also happens to reduce the amount of general disruption and so produces a further benefit on waiting times.
Likewise if sessions are combined (e.g. running one all-day operating list, instead of two half-day lists a few days apart) then there is a small benefit for longwaits and rebookings. This benefit is partially offset because there is a slight increase in the delay to cancelled urgent patients as a result of the less-frequent sessions. Again, combining sessions would normally be considered because of other motivations, namely making it easier to schedule long procedures flexibly, which is why all-day sessions are beneficial in specialties like orthopaedics that have common, long procedures.
For full details of our research into the causes and effects of disruption, see Research White Paper 3. For quantification of their effects on waiting times, see Research White Paper 5 and the updated formula, or use Gooroo Planner for bulk analysis.
